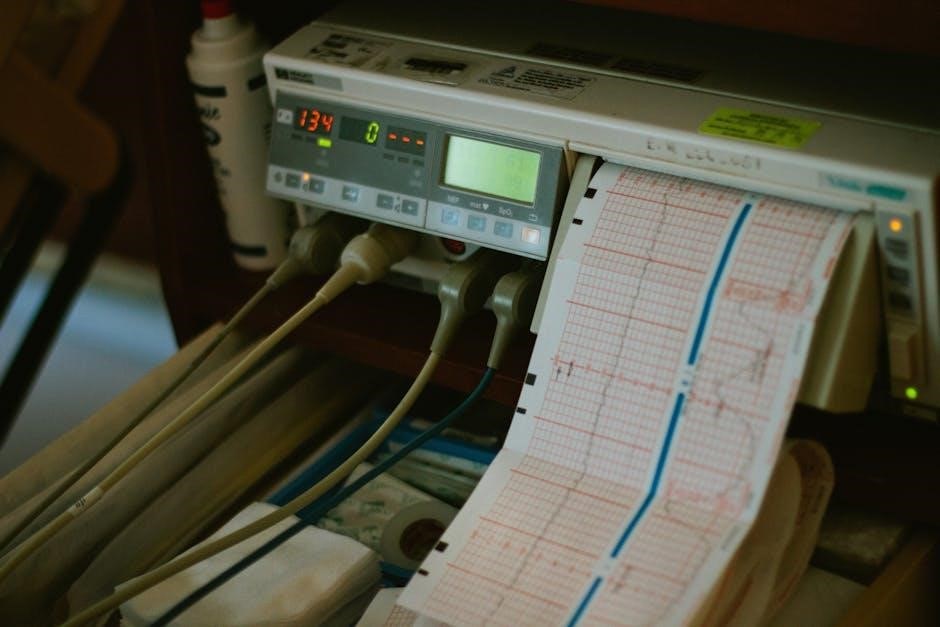
Accurate 12-Lead ECG placement is crucial for diagnosing cardiac issues; this guide provides essential information for healthcare professionals seeking to improve their skills.
Importance of Accurate Placement
Precise electrode placement is paramount in obtaining a reliable 12-Lead ECG, directly impacting diagnostic accuracy. Incorrect positioning can mimic myocardial infarction or obscure genuine changes, leading to misdiagnosis and potentially inappropriate treatment. The AHA emphasizes distal placement on limbs, not strictly wrists or ankles, highlighting the need for consistent technique.
Errors, like limb lead reversals, are common but significantly alter ECG interpretation. Mastering proper placement minimizes artifacts and ensures the ECG accurately reflects the heart’s electrical activity. This skill benefits all healthcare providers, from EMTs in prehospital settings to clinicians in hospitals, enabling timely and effective cardiac care. A solid understanding of placement protocols is therefore non-negotiable for patient safety.
Overview of the 12-Lead System
The 12-Lead ECG system provides a comprehensive view of the heart’s electrical activity from multiple angles. It utilizes ten electrodes – four limb leads (RA, LA, LL, RL) and six precordial (chest) leads (V1-V6) – to create twelve distinct “views” or leads. These leads assess different areas of the heart, enabling detection of various arrhythmias and ischemic changes.
Understanding the spatial relationship of these leads is key to accurate interpretation. Limb leads assess the frontal plane, while precordial leads view the heart in the horizontal plane. Resources like the British Journal of Nursing and online training modules offer detailed diagrams and explanations. Mastering this system requires familiarity with lead positions, color coding, and troubleshooting common placement issues for optimal diagnostic results.
Clinical Significance of ECGs
Electrocardiograms (ECGs) are indispensable tools in modern medicine, offering critical insights into cardiac function. Accurate ECG interpretation, reliant on correct 12-lead placement, aids in diagnosing a wide spectrum of conditions – from life-threatening arrhythmias to subtle signs of myocardial infarction. Paramedics and EMTs heavily depend on ECGs in both prehospital and hospital settings.
Misdiagnosis due to improper lead placement can have severe consequences, potentially leading to false positives or negatives. Therefore, adherence to standardized protocols, like those recommended by the American Heart Association, is paramount. Proper technique minimizes artifacts and ensures reliable data, ultimately improving patient care and outcomes. Continuous education and reference to expert guides are essential.

Understanding ECG Leads and Their Views
Twelve-lead ECGs provide a comprehensive view of the heart’s electrical activity, utilizing limb and precordial leads for detailed diagnostic information.
Limb Leads: I, II, III
Limb leads – I, II, and III – form Einthoven’s triangle, providing a foundational view of cardiac electrical activity. Lead I measures the potential difference between the right and left arms, offering insight into overall cardiac rhythm. Lead II, observing the right arm to the left leg, is frequently used due to its strong signal and consistent view of the heart’s electrical axis. Lead III, spanning the left arm to the left leg, completes the triangle, offering a complementary perspective.
Correct placement of these leads, distal to the shoulder and hip joints (though wrist and ankle placement is also acceptable per AHA guidelines), is vital for accurate readings. Reversals can significantly alter interpretations, potentially leading to misdiagnosis. Understanding the anatomical basis of these leads is essential for effective ECG analysis and patient care.
Augmented Limb Leads: aVR, aVL, aVF
Augmented limb leads – aVR, aVL, and aVF – provide a unipolar view of the heart’s electrical activity, focusing on specific areas. aVR observes the right arm, offering a reversed perspective often useful in identifying right atrial enlargement or conduction abnormalities. aVL views the left arm, aiding in the detection of left atrial issues and lateral wall infarctions. aVF, observing the left foot, provides insight into the inferior wall of the heart.
These leads are created by manipulating the signals from the limb leads, amplifying the voltage. Proper placement, alongside I, II, and III, is crucial for a comprehensive ECG assessment. Errors in placement can mimic pathological findings, emphasizing the need for meticulous technique and understanding of their clinical significance.
Precordial (Chest) Leads: V1-V6
Precordial leads (V1-V6) offer detailed views of the heart’s anterior, lateral, and inferior walls. V1, placed at the fourth intercostal space, right sternal border, assesses septal activity. V2, similarly positioned on the left sternal border, provides a complementary view. V3 and V4, placed between V2 and V4, focus on the anterior wall.
V5, located at the anterior axillary line, and V6, at the mid-axillary line, evaluate the lateral wall. Accurate placement is paramount; even slight deviations can alter interpretations. These leads are vital for identifying ST-segment changes indicative of myocardial ischemia or infarction, making precise positioning essential for reliable diagnosis and patient care.

Electrode Preparation and Skin Considerations
Optimal ECG readings depend on thorough skin preparation and quality electrodes, ensuring strong contact and minimizing interference for accurate cardiac assessments.
Skin Cleaning Protocols
Effective skin preparation is paramount for obtaining a clear and reliable ECG tracing. Prior to electrode application, the skin surface must be thoroughly cleansed to remove oils, dirt, and dead skin cells that can impede electrical conductivity.
Generally, cleaning begins with a dry wipe to remove loose debris, followed by a specialized skin prepping solution – often containing alcohol – applied with a circular motion. Allow the solution to air dry completely before proceeding.
Avoid using lotions or powders, as these can create a barrier and interfere with signal transmission. For patients with excessive skin oils or perspiration, a more aggressive cleaning protocol may be necessary, potentially involving a mild abrasive pad.
Always follow institutional guidelines and consider patient sensitivities when selecting cleaning agents.
Abrasion Techniques for Optimal Contact
When skin preparation alone doesn’t yield a strong signal, gentle abrasion can significantly improve electrode contact. This process removes the outermost layer of dead skin cells, revealing viable tissue with better electrical conductivity.
Utilize a specialized abrasion pad, designed for medical use, and apply light, circular motions to the designated electrode site. Avoid excessive pressure or prolonged abrasion, as this can cause skin irritation or breakdown.
The goal is to create a slightly roughened surface, not to cause bleeding or discomfort. After abrasion, re-clean the area with an alcohol wipe to remove any debris generated during the process.
Always assess the patient’s skin integrity before and after abrasion, and document any adverse reactions.
Electrode Types and Quality
Various electrode types are available, each with unique characteristics impacting signal quality. Standard disposable electrodes consist of a conductive gel sandwiched between a substrate and an adhesive layer. Silver/silver chloride (Ag/AgCl) electrodes are preferred for their low impedance and stable readings.
Cloth electrodes, while reusable, require thorough cleaning and disinfection between patients to prevent cross-contamination. Electrode quality is paramount; expired or poorly manufactured electrodes may exhibit inadequate conductivity or adhesion.
Inspect each electrode package for damage before use, and ensure the gel appears moist and evenly distributed. Proper storage, away from extreme temperatures and direct sunlight, is crucial for maintaining electrode integrity.
Choosing high-quality electrodes contributes significantly to accurate ECG recordings.

Step-by-Step Limb Lead Placement
Correct limb lead placement—right arm, left arm, left leg, and right leg—is fundamental for a reliable 12-lead ECG, ensuring accurate cardiac readings.
Right Arm (RA) Lead Placement
Begin by identifying the right arm. The red electrode, designated for the Right Arm (RA) lead, should be placed on the fleshy part of the right arm, between the shoulder and elbow. Avoid placing it directly over bone or muscle. Ensure good skin contact by gently pressing the electrode onto the prepared skin surface – cleaning and potentially light abrasion are key for optimal signal transmission.
Positioning should be distal to the acromion process, but not directly on it. Consistent placement is vital; slight variations can impact ECG interpretation. The AHA recommends placement on the arm, not necessarily the wrist, though both are acceptable if consistent. Secure the lead firmly to prevent movement during the recording process, as motion artifact can compromise the ECG quality. Proper RA lead placement establishes a crucial positive reference point for the entire 12-lead system.
Left Arm (LA) Lead Placement
Identify the left arm for the next electrode placement. The yellow electrode, representing the Left Arm (LA) lead, is applied to the fleshy portion of the left arm, situated between the shoulder and elbow – mirroring the RA lead’s positioning. As with the RA lead, avoid direct contact with bone or prominent muscle structures to ensure a clear signal.
Consistent placement, distal to the acromion process, is paramount for accurate readings. The AHA guidelines support placement on the arm itself, offering flexibility beyond the wrist, provided consistency is maintained. Secure the electrode firmly to minimize movement and prevent artifact. The LA lead, alongside the RA lead, forms the basis for the limb lead measurements, crucial for identifying cardiac abnormalities. Proper LA placement contributes significantly to a reliable ECG tracing.
Left Leg (LL) Lead Placement
Locate the left leg for the final limb lead placement. The green electrode, designated for the Left Leg (LL) lead, is applied to the fleshy portion of the left leg, also positioned between the hip and ankle, mirroring the RA and LA placements. Avoid bony prominences and muscle mass for optimal signal acquisition. AHA recommendations emphasize placement on the leg itself, offering flexibility beyond the ankle, prioritizing consistent positioning.
Secure the electrode firmly to minimize patient movement and artifact interference. The LL lead, in conjunction with the RA and LA leads, completes the Einthoven’s triangle, forming the foundational limb lead measurements. Accurate LL placement is vital for a comprehensive and reliable ECG interpretation, aiding in the accurate diagnosis of cardiac conditions. Consistency is key for comparable readings.
Right Leg (RL) Lead Placement ౼ Grounding
The Right Leg (RL) electrode, typically white or gray, serves as the ground, minimizing electrical interference and ensuring signal clarity. Position this electrode on the fleshy portion of the right leg, between the hip and ankle, similar to the other limb leads. It’s crucial to avoid bony areas or muscle mass for optimal contact and signal quality. The RL lead doesn’t directly contribute to the ECG waveform but is essential for a stable baseline.
Proper grounding reduces artifact from muscle activity and external sources. AHA guidelines suggest placement on the leg itself, allowing flexibility beyond the ankle. Secure the electrode firmly to the skin, ensuring consistent contact throughout the recording. A well-grounded RL lead is fundamental for accurate ECG interpretation and reliable cardiac assessments, preventing misleading results.
Detailed Precordial Lead Placement
Precise placement of V1-V6 is vital for accurate diagnosis; follow standardized protocols for optimal visualization of cardiac electrical activity and reliable results.
V1 Placement – Fourth Intercostal Space, Right Sternal Border
V1 is positioned in the fourth intercostal space, directly on the right sternal border. This location provides a view of the atrial activity and the right ventricle. Proper placement ensures accurate detection of potential right ventricular hypertrophy or conduction abnormalities. It’s essential to palpate the intercostal spaces to confirm correct positioning, avoiding common errors like placement too high or too low.
Careful attention to anatomical landmarks is key. Incorrect V1 placement can mimic or obscure true pathology, leading to misdiagnosis. Consistent technique and adherence to guidelines are paramount for reliable ECG interpretation. Remember to prepare the skin adequately for optimal electrode contact and signal quality.
V2 Placement – Fourth Intercostal Space, Left Sternal Border
V2 is strategically placed in the fourth intercostal space along the left sternal border. This lead offers a crucial perspective on the left atrium and the anterior wall of the left ventricle. Accurate positioning is vital for identifying signs of left ventricular hypertrophy, septal infarction, or bundle branch blocks. Palpate carefully to confirm the fourth intercostal space, avoiding common placement errors that can distort the ECG tracing.
Consistent technique and adherence to standardized protocols are essential. Proper skin preparation enhances electrode contact and signal quality. Misplacement can lead to inaccurate interpretations, potentially delaying appropriate treatment. Always double-check the lead’s position before initiating the ECG recording to ensure reliable diagnostic information.
V3 & V4 Placement – Between V2 & V4
V3 and V4 are positioned midway between V2 and V4, typically in the fourth intercostal space. V3 is placed directly on the anterior midline, while V4 resides in the fifth intercostal space at the midclavicular line. These leads provide critical views of the anterior and septal walls of the left ventricle, aiding in the detection of anterior myocardial infarction and left ventricular hypertrophy.
Precise placement is paramount; errors can mimic or obscure true pathology. Palpate intercostal spaces carefully to ensure accuracy. Consistent technique and proper skin preparation are vital for optimal signal quality. Always verify lead positions before recording to avoid misinterpretations and ensure reliable diagnostic data for effective patient care.
V5 Placement – Fifth Intercostal Space, Anterior Axillary Line
V5 is strategically placed in the fifth intercostal space, at the anterior axillary line. This position offers a lateral view of the heart, specifically focusing on the left ventricle’s lateral wall. It’s crucial for identifying lateral wall ischemia or infarction, as well as assessing left ventricular function. Accurate placement requires careful anatomical landmark identification.
Consistent technique and proper skin preparation are essential for a clear signal. Misplacement can lead to diagnostic errors, potentially masking or mimicking cardiac abnormalities. Always double-check the position before recording, ensuring optimal contact and minimizing artifact. Reliable data is paramount for effective patient assessment and treatment planning.
V6 Placement – Fifth Intercostal Space, Mid-Axillary Line
V6 resides in the fifth intercostal space, positioned at the mid-axillary line, providing a further lateral perspective of the left ventricle. This lead is particularly sensitive to changes indicative of lateral wall ischemia, infarction, or hypertrophy. Precise placement is vital for accurate diagnosis and effective patient care.
Ensure proper skin preparation and electrode adhesion to minimize artifact and obtain a clear signal. Incorrect positioning can significantly alter the ECG tracing, leading to misinterpretations. Consistent technique and anatomical landmark verification are key. A well-placed V6 contributes significantly to a comprehensive cardiac assessment, aiding in timely and appropriate interventions.

Common Placement Errors and Artifacts
Errors like limb lead reversals or incorrect precordial positioning are frequent; recognizing and minimizing artifacts—muscle tremor, wandering baseline—is vital for accurate readings.
Limb Lead Reversals
Limb lead reversals represent a significant, yet surprisingly common, error in 12-lead ECG acquisition. Most frequently, the right and left arm leads are transposed, dramatically altering the ECG tracing and potentially leading to misdiagnosis. Specifically, a right arm (RA) and left arm (LA) swap effectively inverts leads I and aVR, while simultaneously swapping the polarity of aVL and aVF.
This can mimic acute myocardial infarction or obscure existing ischemic changes. Recognizing this error requires careful assessment of the ECG; look for an inverted P wave and QRS complex in lead I, alongside corresponding changes in aVR. Prompt identification and correction are paramount to avoid incorrect clinical decisions. Consistent training and double-checking lead placement are essential preventative measures.
Incorrect Precordial Lead Positioning
Improper placement of precordial (chest) leads significantly impacts ECG accuracy, often mimicking or masking true pathology. Shifting a lead even one intercostal space can alter the recorded electrical activity, leading to false-positive or false-negative interpretations for myocardial infarction. For instance, displacing V3 and V4 too high can simulate left ventricular hypertrophy, while positioning them too low may suggest inferior wall ischemia.
Consistent adherence to anatomical landmarks – intercostal spaces and sternal/axillary lines – is vital. Careful attention to patient anatomy, particularly in individuals with unusual chest wall configurations, is also crucial. Regular quality control checks and standardized protocols minimize these errors, ensuring reliable ECG data for accurate diagnosis and treatment.
Identifying and Minimizing Artifact
ECG artifact, interference obscuring the true electrical signal, commonly arises from patient movement, muscle tremor, or external sources. Recognizing artifact is crucial to avoid misinterpretation. Baseline wander, appearing as a drifting line, often stems from respiration or poor electrode contact. Muscle tremor presents as rapid, erratic deflections, particularly in limb leads.
Minimizing artifact involves meticulous skin preparation – cleaning and gentle abrasion – to enhance electrode adhesion. Patient instruction to remain still during recording is essential. Filtering options on ECG machines can reduce certain frequencies of interference, but should be used cautiously. Identifying and addressing the source of artifact ensures a clear, interpretable ECG tracing.

Troubleshooting ECG Placement Issues
Addressing signal quality problems, wandering baselines, and muscle tremor requires careful electrode assessment, patient repositioning, and potential adjustments to recording settings.
Poor Signal Quality – Causes and Solutions
Identifying the root cause of poor signal quality is paramount for obtaining a diagnostic ECG. Common culprits include inadequate skin preparation, leading to high impedance and weak signal transmission. Ensure thorough skin cleaning and abrasion to optimize electrode contact.
Loose or damaged electrodes, and cables can also contribute to signal degradation. Regularly inspect all components for wear and tear, replacing as needed. Patient factors, such as excessive muscle movement or shivering, introduce artifact.
Environmental interference from electrical devices can also impact signal clarity. Minimize these sources if possible. Solutions involve re-applying electrodes, adjusting the ECG machine’s gain settings, and ensuring proper grounding. If issues persist, consider alternative lead placement or exploring underlying patient conditions.
Wandering Baseline – Identification and Correction
A wandering baseline on an ECG appears as a drifting of the isoelectric line, obscuring accurate waveform interpretation. This is frequently caused by patient movement – breathing, talking, or even subtle shifts in position – introducing artifact. Poor electrode contact and inadequate skin preparation can exacerbate the issue, increasing impedance and susceptibility to interference.
Identifying a wandering baseline involves visually inspecting the ECG tracing for consistent upward or downward drift. Correction strategies begin with ensuring patient stability and minimizing movement.
Re-applying electrodes with firm contact and optimizing skin preparation are crucial. Adjusting the ECG machine’s baseline correction settings can also help stabilize the tracing. If the problem persists, consider utilizing filters, but cautiously, as they can distort the signal.
Muscle Tremor Artifact – Reduction Techniques
Muscle tremor artifact manifests as rapid, irregular spikes or waves on the ECG, mimicking cardiac activity and potentially leading to misdiagnosis. This is commonly caused by patient shivering, anxiety, or even subtle muscle contractions. Proper patient positioning and reassurance are the first steps in minimizing this interference.
Ensuring firm electrode contact and thorough skin preparation are vital; loose electrodes amplify muscle activity. Instructing the patient to remain still and breathe slowly can significantly reduce tremors.
Applying gentle pressure around the electrode sites can help stabilize them. If artifact persists, consider adjusting the ECG machine’s filtering settings, but be mindful of potential signal distortion; In severe cases, re-application of electrodes may be necessary.

Resources and Further Learning
Explore AHA guidelines, online modules, and medical journals for in-depth knowledge of 12-lead ECGs and proper placement techniques for accurate readings.
American Heart Association (AHA) Guidelines
The American Heart Association (AHA) provides foundational guidance for standardized 12-lead ECG placement, emphasizing consistent technique for reliable interpretation. Their 1975 statement recommended distal limb electrode placement – beyond the shoulders and hips – though not strictly limited to wrists and ankles.
AHA recommendations focus on minimizing artifacts and ensuring clear signal acquisition. Proper placement, as outlined by the AHA, is vital for accurate diagnosis of cardiac dysrhythmias and conditions like myocardial infarction. Adhering to these guidelines reduces the risk of misinterpretation and supports effective patient care.
Further resources from the AHA include educational materials and updates on best practices, continually refining standards for optimal ECG acquisition and analysis. Consistent application of AHA guidelines is paramount for all healthcare professionals performing and interpreting 12-lead ECGs.
Online ECG Training Modules
Numerous online ECG training modules offer comprehensive instruction on 12-lead placement, supplementing traditional learning methods. These resources frequently utilize interactive diagrams and video demonstrations to illustrate correct electrode positioning and common pitfalls; Many modules emphasize step-by-step procedures, reinforcing proper technique for both limb and precordial leads.
These digital platforms often include quizzes and assessments to evaluate understanding and identify areas needing improvement. They can be particularly valuable for healthcare professionals seeking continuing education or initial training in ECG interpretation and placement. Modules frequently cover artifact recognition and troubleshooting techniques.
Accessible from various devices, these online resources provide flexible learning opportunities, enhancing competency in accurate ECG acquisition and minimizing potential errors in clinical practice. They are a valuable tool for mastering this essential skill.
Relevant Medical Journals and Publications
Peer-reviewed medical journals provide in-depth analyses of ECG placement techniques and their impact on diagnostic accuracy. Publications like the British Journal of Nursing (2019) have specifically addressed the importance of correct lead positioning, highlighting potential consequences of errors, such as false infarction indications. Research articles often detail the effects of subtle placement variations on ECG waveforms.
International journals frequently publish studies on limb lead reversals and other common errors, offering insights into minimizing misinterpretations. These resources also explore advancements in electrode technology and skin preparation protocols. Accessing these publications ensures healthcare professionals remain updated on best practices.
Staying current with the latest research is vital for maintaining competency and delivering optimal patient care. These journals offer evidence-based guidance for accurate ECG acquisition and interpretation.

